Lesson 8: Wide Complex Tachycardia
- Tooba Alwani
- May 14, 2025
- 3 min read
Summary of Learning points
Normal QRS duration = 60-100 msec
Wide QRS = QRS duration > 120 msec (3 little boxes)
Differential diagnosis for wide QRS complex tachycardia:
SVT with permanent BBB (fixed conduction defect block is present at any heart rate)
SVT with rate-dependent BBB (prolonged bundle branch refractory period no block below a critical heart rate, though block manifests at higher HR)
SVT with pre-excitation (accessory pathway)
Accessory pathway allows atrial impulse to bypass AV node
Example: WPW (Wolff-Parkinson-White) accessory pathway causing early depolarization of ventricular tissue close to the insertion of the accessory pathway, which shows up on ECG as a delta wave
Allows for the existence of AVRT, a re-entrant circuit including both the AV node and the accessory pathway
Orthodromic AVRT: narrow QRS complex (impulse travels to the ventricles normally through the AV node, but returns to the atria abnormally through the accessory pathway)
Antidromic AVRT: wide QRS complex (impulse travels to the ventricles abnormally through the accessory pathway, causing initial slow cell-to-cell depolarization leading to wide QRS complex, but returns to the atria via retrograde conduction through the AV node)
VT
Definition: 3 consecutive ventricular depolarizations at a rate > 100 bpm
Ventricular rhythm with rate < 100 bpm = usually AIVR (accelerated idioventricular rhythm)
Can be monomorphic (QRS complexes all the same amplitude) or polymorphic (multiple QRS amplitudes)
Caused by re-entry circuits around areas of prior myocardial scar or by triggered activity (eg the “R-on-T” phenomenon that induces torsades de pointes, a specific subcategory of polymorphic VT)
Common misconceptions:
VT is NOT always fast! Can have rates <150 or even <130 if on antiarrhythmics
VT is NOT always hemodynamically unstable! People can be minimally symptomatic in VT, especially at lower heart rates
Other commonly discussed ECG tricks (precordial concordance, “northwest” or extreme right axis deviation) are useful but not 100% specific even when present
Toxic or metabolic abnormality
Digoxin toxicity, TCA overdose, sodium channel blocker overdose, electrolyte abnormalities
What to do when you see a wide complex rhythm:
Is the patient hemodynamically unstable?
If so, it doesn’t matter what the rhythm is – cardiovert them (AFTER YOU SEDATE THEM) and figure out the rhythm later
Patient factors:
Older, known structural heart dz, prior infarct ischemia more likely VT
Younger, prior BBB with identical morphology to current ECG, evidence of WPW more likely SVT
If unsure, assume VT until proven otherwise
Look in more detail at the ECG!
AV dissociation: P waves and QRS complexes at different frequencies
Can manifest with fusion beats (supraventricular + ventricular beat occurring at the same time weird looking “hybrid” complex) or capture beats (a supraventricular impulse occurs just at the right time to “capture” the ventricles), but these usually only occur at lower heart rates
QRS duration: if QRS duration > 160 ms, more likely VT
Remember to measure the QRS from the earliest start of the QRS complex in any lead to the latest termination of the QRS complex in any lead (even if it’s a different lead!)
Other factors that favor VT:

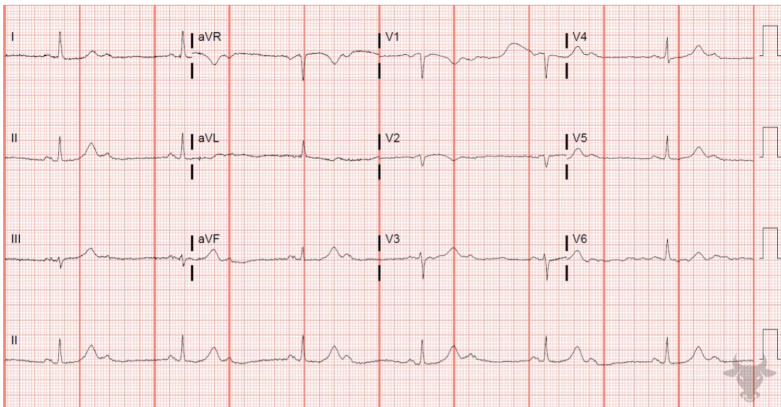
Practice ECG

Answer
Rate: ~140
Rhythm: no discernible p waves, monomorphic
Axis: northwest axis deviation (positive in aVR, negative in II/aVF)
Intervals: very wide QRS (>200 msec) with RBBB morphology (monophasic R wave in V1, slurred S wave in V6)
Other: R:S <1 in V6, RS interval ~180msec in V1, R wave peak time ~60 msec in aVR
Diagnosis: likely monomorphic VT, RBBB pattern